70Y Female With Complaints of Loose Stools since 2 years and Abdominal Pain since 2 Years.
2019 : She was diagnosed with Cholelithiasis, and underwent Cholecystectomy
2021 : She Started having Complaints of pain Abdomen.
Loose stools, and Burning Type of Pain while Passing stools.
Losse stools were Non blood stained, Pale in Colour, Slimy in Consistency.
And Decreased Appetite
She went to a local doctor. No record of it.
December 2021 : Later that year she went to visit her relatives in Mumbai where she went to see a doctor in the hospital for her symptoms on advice of their relatives,
Endoscopy was advised for the Patient.
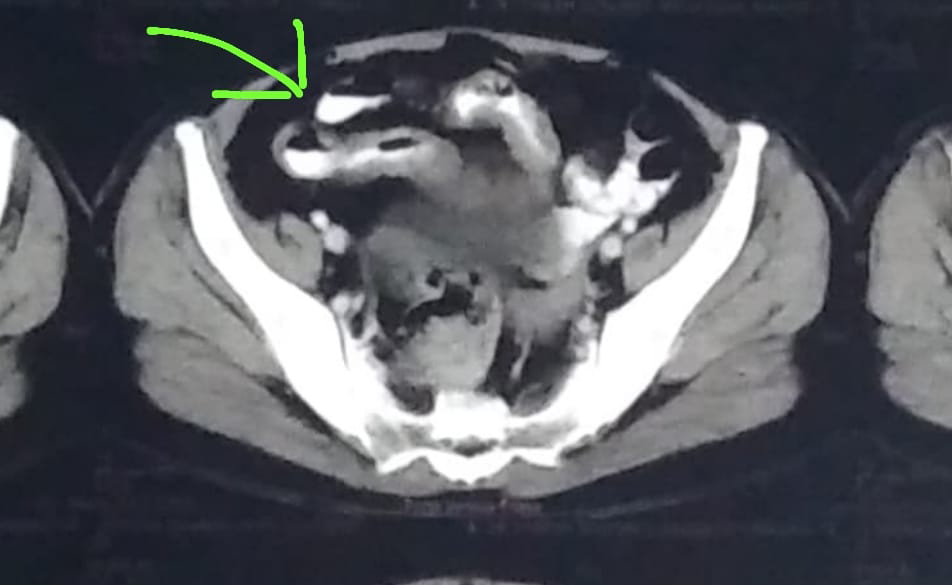
CT SCAN Abdomen was done :
Impression: Diffuse Long segment Mural Thickening along the terminal Ileum
Fatty liver , Borderline Spleenomegaly, Mildly Prominent Common Bile Duct - Post Operative Satus.
Bilateral simple cortical cysts
Few Small Subcentimeter mesenteric lymph nodes.
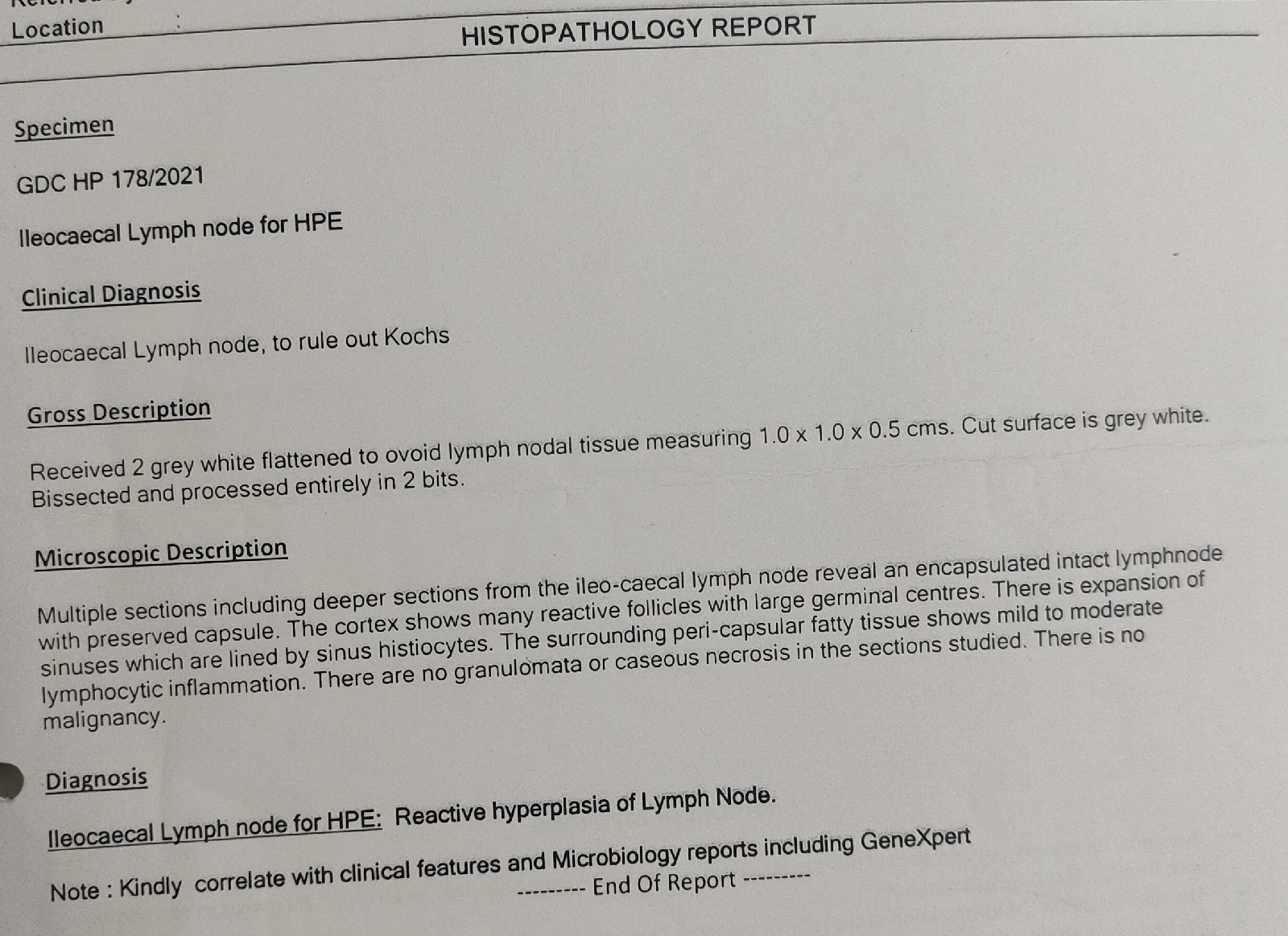
ILIOCAECAL - LYMPH NODE Biopsy was done :
Impression: Reactive Hyperplasia of Lymph node
Rx Given :
Tab Veloz D
Unienzyme Tablet
Cremaffin syrup
2023 : She was Apparently alright until 6 months ago where she started having similar complaints.
She went to see a local Doctor who prescribed her the following medication :
Rx ;
Rifaximin 400
Pre and Probiotic capsules
Raciper D
Vibact DS capsules
Libratex (Chlordiazepoxide and Clidinium)
Cremaffin Syrup
But her symptoms did not improve and She came to this Hospital.
Dec 2023 :
Patient Came to the OPD with chief Complaints of Pain in Abdomen( Just before Passing stools)Since 2 Years
Loose Stools 2-3 episodes per day, Non Blood Stained, Pale in Colour, Watery In Consistency Since 2 Years
Her Abdominal Pain relieved after passing Stools
Past History:
K/C/O Hypertension Since 4 years - On Tab. Amlodipine 2.5 MG Once Daily
Not a K/C/O DM, Asthma, CVA, CAD, Epilepsy, Thyroid Disorders.
H/O Cholelithiasis 4 Years Back - Underwent Cholecystectomy Surgery.
Underwent Iliocaecal lymph node biopsy 2 years Back Showing : Reactive Hyperplasia of lymph node.
Personal History:
Diet : Mixed
Appetite: Decreased
Bowel : Irregular
Micturition : Nomal
Addictions: Use of Betel Leaf(Pan) For Past Years.
Family History:
No Significant Family History
General Examination:
Pallor is Present
No Features indicating the presence of Icterus, Clubbing, Pedal Edema, Lymphadenopathy.
Vitals :
Temperature - 98.2 °F
PR - 84 BPM
RR - 16 CPM
BP - 120/80 mmHg
GRBS - 142 mg/dl
Systemic Examination :
Abdominal Examination:
Inspection:
No Distension
Scar of Surgery for Intestinal Obstruction and Iliocaecal lymph node biopsy seen.
Umbilicus - Inverted
Equal Symmetrical Movements in all the Quadrants with respiration.
No visible Pulsations, Peristalsis, Dilated Veins, and Localised Swellings.
Palpation :
No Local Rise of Temperature, Abdomen is Soft With No Tenderness.
Auscultation :
Bowel Sounds Present.
CVS - S1, S2 Heart Sounds Heard. No murmurs.
RS : Bilateral Air Entry Present, Normal Vesicular Breath Sounds Heard.
CNS Examination: No Focal Neurological Deficits.
Provisional Diagnosis:
Inflammatory Bowel Disease
Investigations:
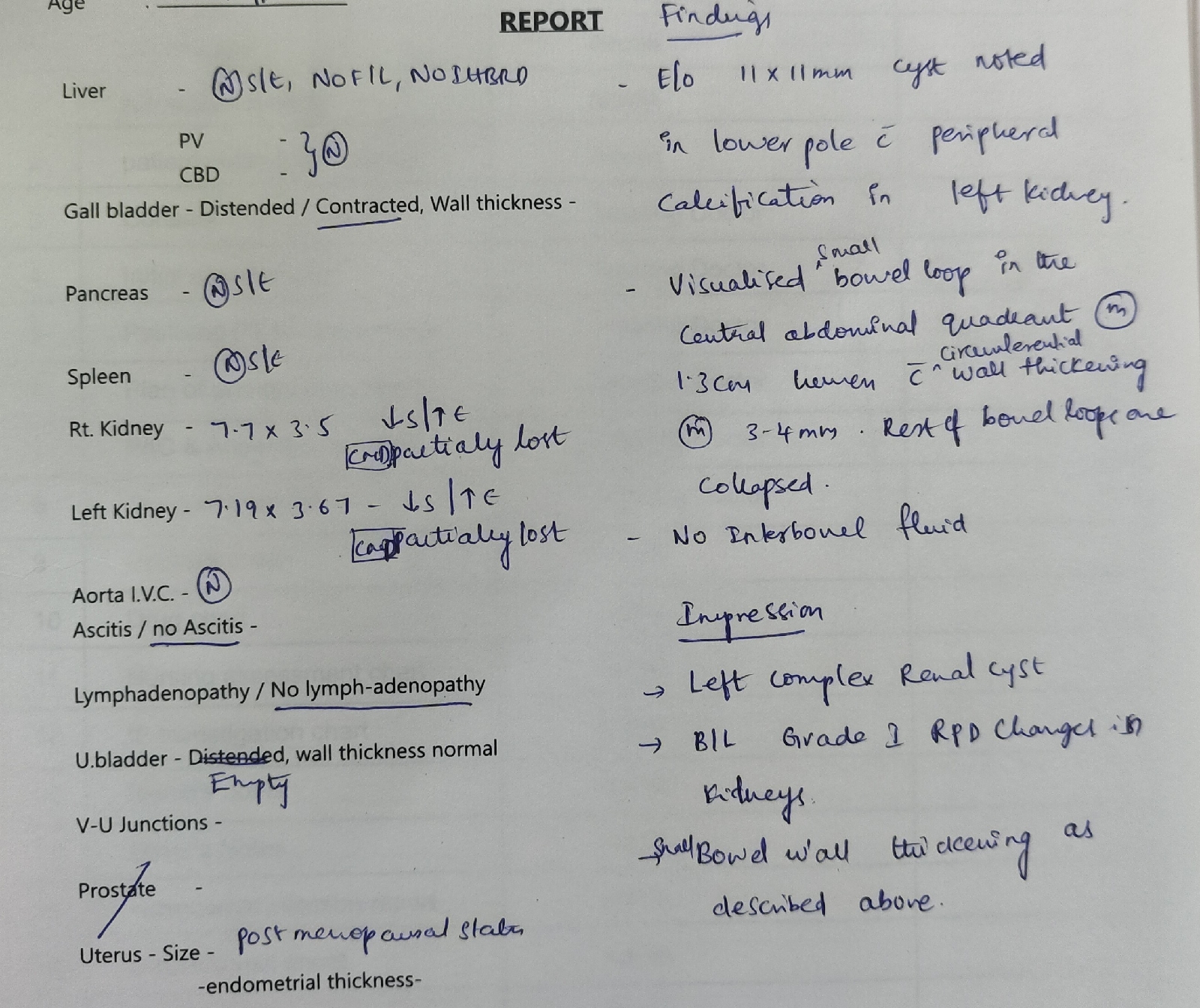
USG abdomen and Pelvis:
Treatment:
1. Tab. Rifaximin 400 MG PO/OD
2. Tab. Amlodipine 2.5 MG PO/OD
SOAP NOTES :
20/12/23
S:
No complaints of fever.
2 Episodes of loose stools.
O:
Patient is conscious, coherent and cooperative
Temp: 98.2 °F
Bp: 120/80 mmHg
PR: 84 bpm, regular
RR: 16 cpm
GRBS: 142 mg/dl
CVS: S1 S2+ , no murmurs heard
RS: Bilateral air entry+, NVBS heard
CNS: NFND
P/A: Soft, No Tenderness Present, bowel sounds heard
A:
Inflammatory Bowel Disease.
P:
1. Tab. Rifaximin 400 MG PO/OD
2. Tab. Amlodipine 2.5 MG PO/OD
21/12/23
S:
No New Complaints,
No complaints of fever.
2 Episodes of Passing stools. Yellowish in Colour and normal in Consistency.
O:
Patient is conscious, coherent and cooperative
Temp: 98.4°F
Bp: 130/80 mmHg
PR: 88 bpm, regular
RR: 16 cpm
GRBS: 106 mg/dl
CVS: S1 S2+ , no murmurs heard
RS: Bilateral air entry+, NVBS heard
CNS: NFND
P/A: Soft, No Tenderness Present, bowel sounds heard
A:
Inflammatory Bowel Disease.
P:
1. Tab. Rifaximin 400 MG PO/OD
2. Tab. Amlodipine 2.5 MG PO/OD
22/12/23
S:
No New Complaints,
No complaints of fever.
1 Episode of Passing stools. Yellowish in Colour and normal in Consistency.
O:
Patient is conscious, coherent and cooperative
Temp: 98.4°F
Bp: 120/80 mmHg
PR: 76 bpm, regular
RR: 16 cpm
CVS: S1 S2+ , no murmurs heard
RS: Bilateral air entry+, NVBS heard
CNS: NFND
P/A: Soft, No Tenderness Present, bowel sounds heard
A:
Inflammatory Bowel Disease.
P:
1. Tab. Rifaximin 400 MG PO/OD
2. Tab. Amlodipine 2.5 MG PO/OD
23/12/23
S:
No New Complaints,
No complaints of fever.
1 Episode of Passing stools. Yellowish in Colour and normal in Consistency.
O:
Patient is conscious, coherent and cooperative
Temp: 98.4°F
Bp: 120/80 mmHg
PR: 76 bpm, regular
RR: 16 cpm
CVS: S1 S2+ , no murmurs heard
RS: Bilateral air entry+, NVBS heard
CNS: NFND
P/A: Soft, No Tenderness Present, bowel sounds heard
A:
Inflammatory Bowel Disease.
P:
1. Tab. Rifaximin 400 MG PO/OD
2. Tab. Amlodipine 2.5 MG PO/OD









Comments
Post a Comment