A 70 Year Old Male With Breathlessness and Decreased Appetite
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Ankur Kumar
CASE REPORT :
A 70 Year Old Male Patient, Agricultural Labourer by occupation, Presented with Chief Complaints of Breathlessness and Decreased Appetite Since 4 Days.
Patient came to the hospital 6 months ago with chief complaints of high grade fever insidious in onset that is associated with chills and rigors, intermittent type relived with medication. Later he developed Generalized weakness insidious in onset which led to his inability to perform his daily activities and was brought to hospital.
There was H/O Giddiness, H/O Fall (Twice), H/O Loss of Consciousness for 5 min.
Reference : https://maheshwarijagathkari57.blogspot.com/2023/06/66-year-old-with-high-grade-fever-and.html
Patient came to the hospital again as 4 Days ago then he developed Breathlessness insidious in onset Gradually Progressive, exaggerated after food intake and relieved with rest.
Patient has a History of fall in the Bathroom one week ago.
Decreased Appetite Since 4 Days.
No H/O Cough, Cold, Fever
No H/O Abdominal Pain / Burning Micturition
No H/O Chest Pain, Palpitations, Loose motions, Profuse Swellings.
PAST HISTORY :
K/C/O HbsAg Positive On Treatment
K/C/O DM Since 20 Years on Treatment ( Inj. HAI)
K/C/O Hypertension on Treatment
K/C/O CVA (Acute Infarct in Right Frontal Lobe) on Treatment (Antiplatelets)
K/C/O CKD ( Stage - III )
Left Lower Limb and Scrotum Filariasis on Treatment
Personal History :
Diet - Mixed
Appetite - Decreased
Bowel and Bladder - Normal
Addictions - Consumed Alcohol Everyday ,
1-2 pegs daily for past 4 years.
Smoked a pack of beedis a day, Quit 7 years ago.
Family History:
No Significant Family History
General Examination:
Pallor is Present
Pedal Edema is Present
No features indicating the presence of icterus, cyanosis, clubbing, lymphadenopathy.
Pedal Edema in Right Lower Limb
Left Lower Limb with Filariasis
Pics
6Months (June) ago Vs Today( November)
Patient has lost significant Muscle mass in the past 6 months.
Vitals :
Temperature - 98.4 F
PR - 86/min
RR - 17 CPM
BP - 140/80 mmHg
SpO2 - 77% at RA.
98% with 10 lit. of O2
SYSTEMIC EXAMINATION :
ABDOMINAL EXAMINATION :
INSPECTION :
No distention, No scars
Umbilicus - Inverted
Equal symmetrical movements in all the quadrants with respiration.
No visible pulsation, peristalsis, dilated veins and localized swellings.
PALPATION :
No local rise of temperature, Abdomen is soft with no tenderness.
No spleenomegaly, hepatomegaly
PERCUSSION
Liver span is 12cm, No hepatomegaly
Fluid thrill and shifting dullness absent.
No puddle sign.
AUSCULTATION
Bowel sounds present.
CVS- S1 and S2 heart sounds heard.
RS- Bilateral air entry is present, normal vesicular breath sounds heard.
RS : BAE +
Crepts present in the
Right - MA, IAA, ISA
Left - MA, ISA
CNS EXAMINATION
Right Handed person, uneducated
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, Coherent, Cooperative
Speech : Muffled, Not Clear
Behaviour : Normal
Memory : Intact.
Intelligence : Normal
No hallucinations or delusions.
CRANIAL NERVE EXAMINATION: Intact
MOTOR EXAMINATION:
Right. Left
POWER
UL 4/5 O/5
LL 4/5. 3/5
REFLEXES
Right Left
BICEPS +++ ++
TRICEPS ++ +
SUPINATOR +++ ++
KNEE +++ +++
ANKLE ++ ++
PLANTAR. Flexor flexor
SENSORY EXAMINATION: Intact
PROVISIONAL DIAGNOSIS:
Hypertension
Diabetes Mellitus
Chronic Kidney Disease Stage III
CVA ( SubAcute Infarct in Right Frontal Lobe)
HbsAg Positive
Left Lower Limb Elephantiasis
INVESTIGATIONS :
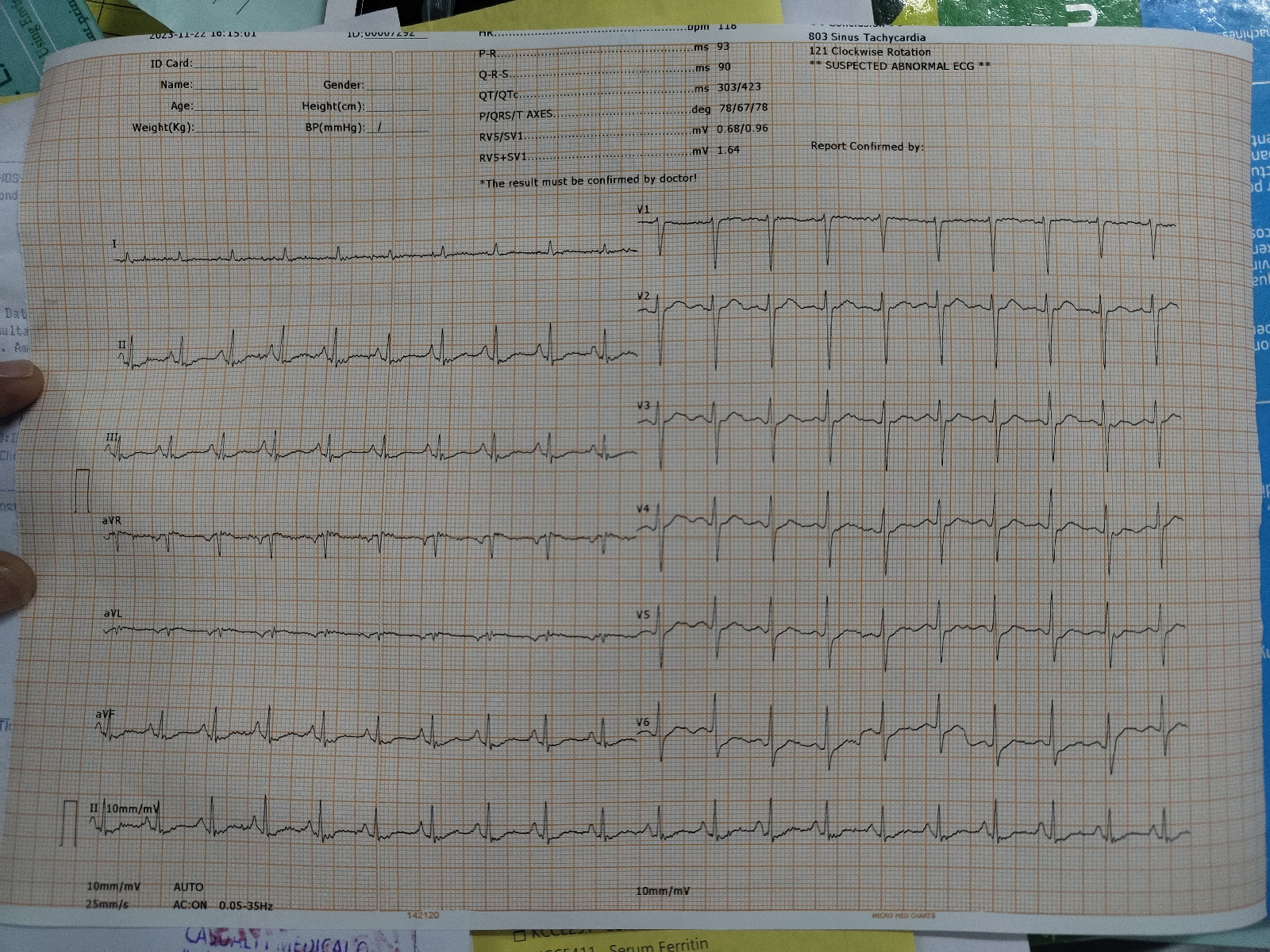
ECG :
X Ray Chest
X- Ray C - Spine
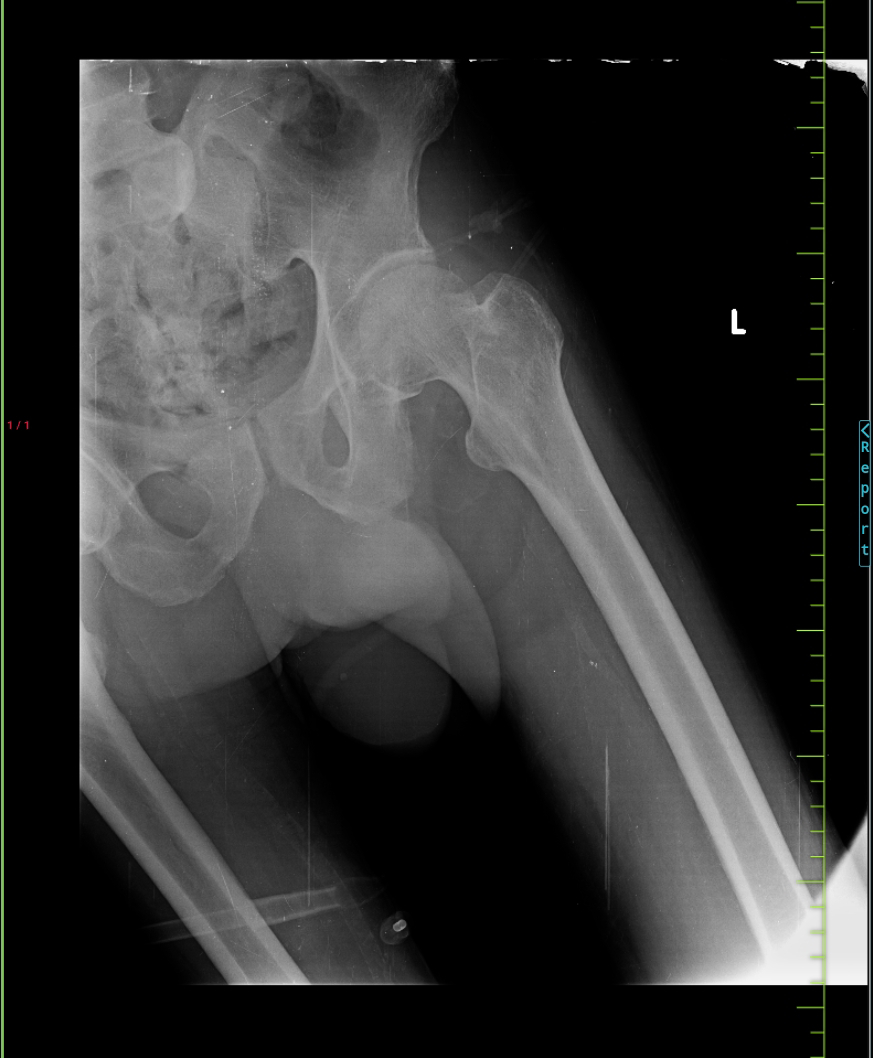
X-Ray
Serology:
HbsAg - Positive
HIV. - Negative
HCV - Negative
USG :
23/11/23
Hemogram :
LIPID PROFILE :
Fasting Blood Sugar - 216mg/dl
RFT :
24/11/23
CT BRAIN
Hemogram
RFT
Serum electrolytes :
Serum Magnesium - 2.1 mg/dl
Urinary Electrolytes :
Urinary Chloride - 189 mmol/L
Urinary Sodium - 148 mmol/L
Urinary Potassium - 23.02
25/11/23
RFT
Hemogram
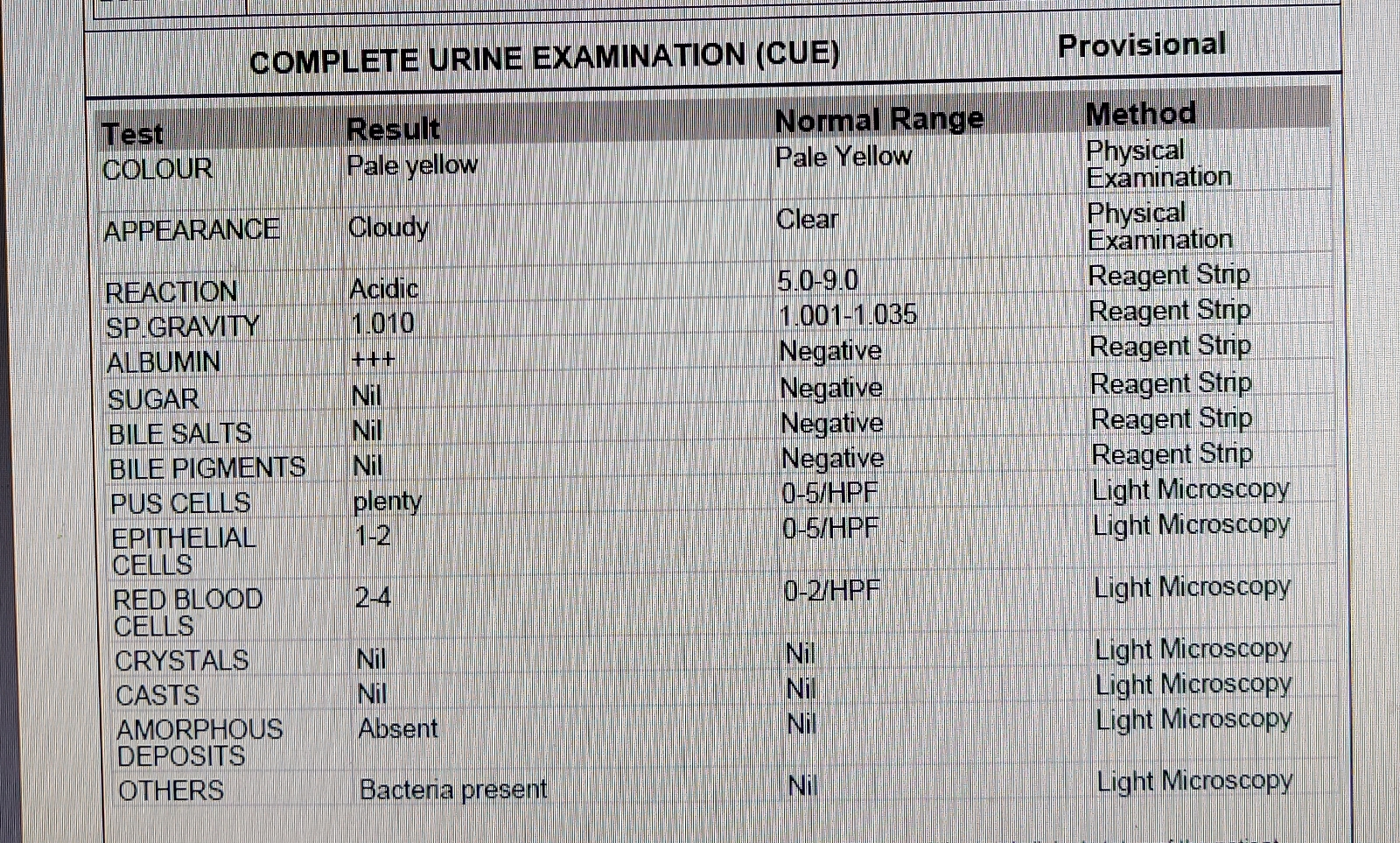
Complete Urine examination
ESR
26/11/23
Hemogram
RFT
CUE
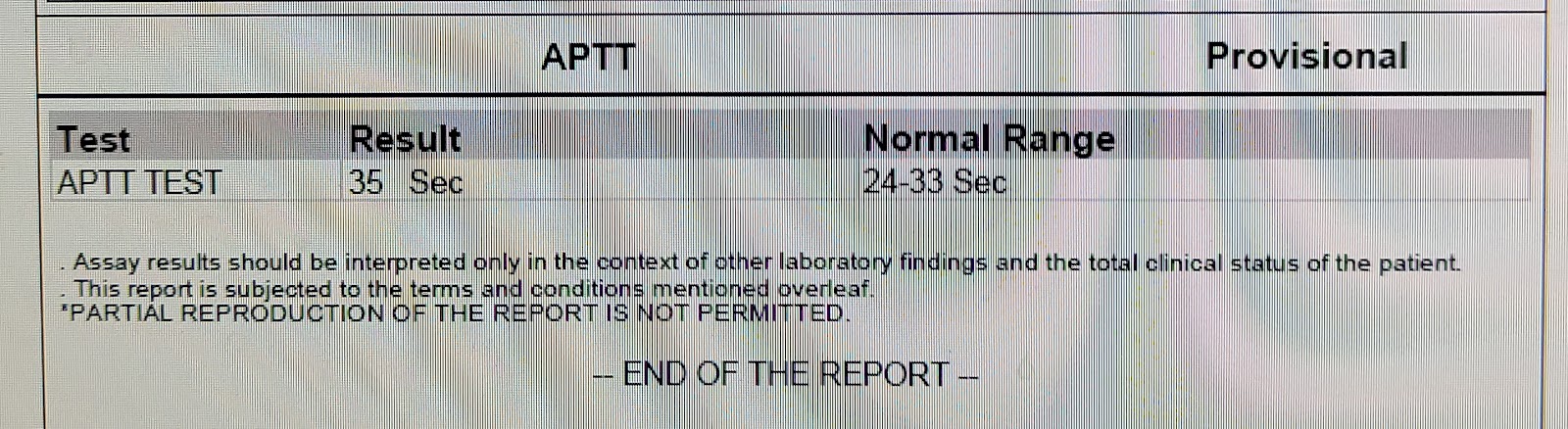
APTT
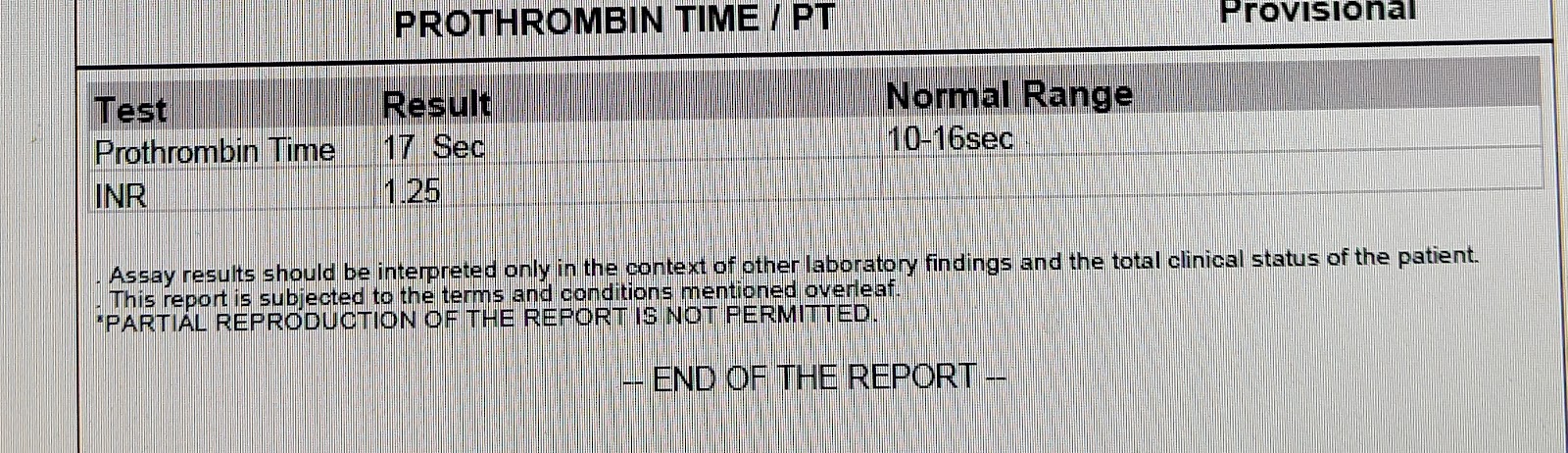
PT
27/11/23
CT ABDOMEN
CBP
COMPLETE URINE EXAMINATION
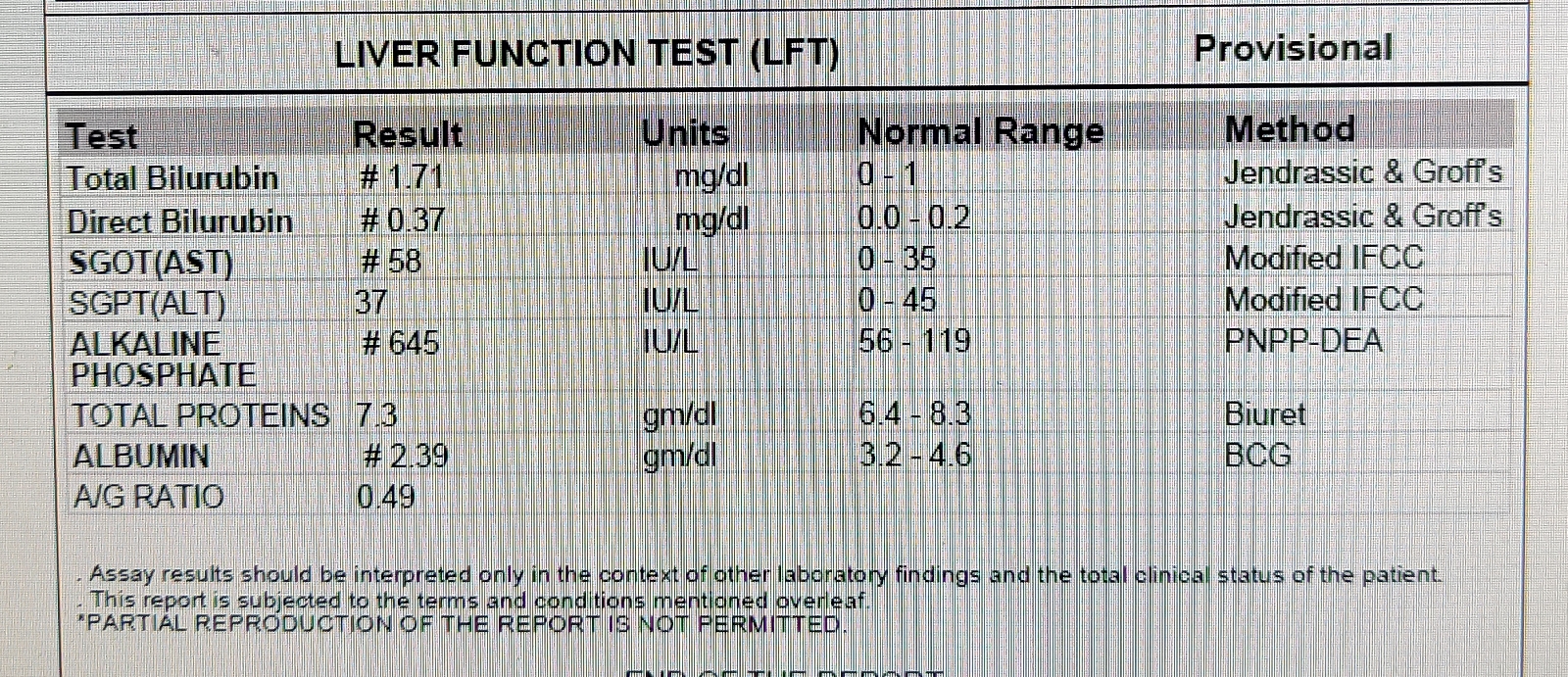
LFT
RFT
Treatment
1) RT feeds water - 100 ml - 2nd hourly, milk - 50ml + Protein powder 3rd hourly.
2) Inj. HAI SC TID (8U-8U-8U)
3) TAB. Lasix 20mg RT/OD
4) Tab. Amiodipine 5 mg RT/OD
5) TAB. Ecospirin 75mg RT/OD
6) Tab. Clopidogrel 75mg RT/OD
7) Tab. Atorvastatin 20mg RT/OD
8) Tab. Orofer xt RT/OD
9) Tab Nodosis 500 mg RT/BD
10) Tab. Shelcal ct RT/OD
11) Cap. Bio- D3 RT/OD
12) Inj. PCM 1gm IV /SOS
13) Syp. Cremaffin 15ml RT/TID






























Comments
Post a Comment